Share this
One Year Later: What if Congress Had Repealed the Affordable Care Act? For too long, too many hard working Americans paid the price for policies that handed free rein to insurance companies with few protections for patients or providers. Nearly two years ago, President Obama signed health reform – the Affordable Care Act – into…
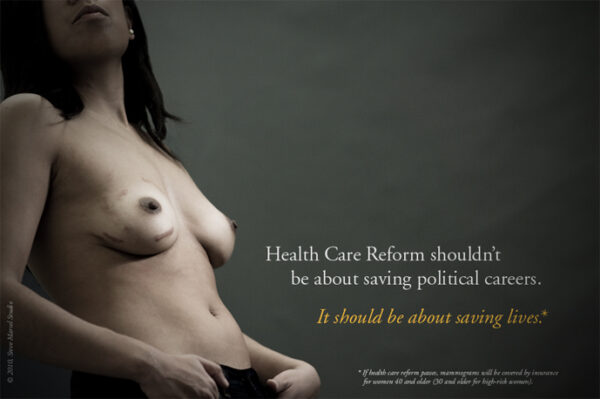
Preventive Services Covered by Private Health Plans Under the ACA The Affordable Care Act created new requirements that private insurers cover preventive services, including routine immunizations, screenings for conditions such as cancer and high cholesterol, and preventive services for women. A new fact sheet from the Kaiser Family Foundation outlines these prevention requirements and discusses…
Brittanie Turpin, 23, accumulated $20,000 in medical debt from emergency gallbladder surgery last year. “It’s pretty tough without insurance,” Turpin said. Under the Affordable Care Act, passed one year ago, Turpin will be able to stay on her mother’s insurance until she is 26. (Brad Nettles) From The Post & Courier: Benefits to S.C. so…
9 Ways The New Law May Affect You in 2011 By Kaiser Health News Staff Jan 03, 2011 Opponents of the new health care overhaul law are threatening to repeal, defund and kill it in court, but that isn’t stopping Washington from implementing a number of important provisions in 2011. While many people will welcome…
Co-payments for many preventive medical services for most workers are about to disappear The new federal healthcare law aims to encourage employees to get routine screenings and checkups that could help lower medical costs. By Bruce Japsen November 1, 2010 If you’ve been holding off getting screened for high cholesterol, diabetes or hypertension because of…
Share this
Contact Us
Have questions? Send us a private message using the form below.